Kickstart Your Path to a Heart-Healthy Life and Keep Coronary Heart Disease at Bay!

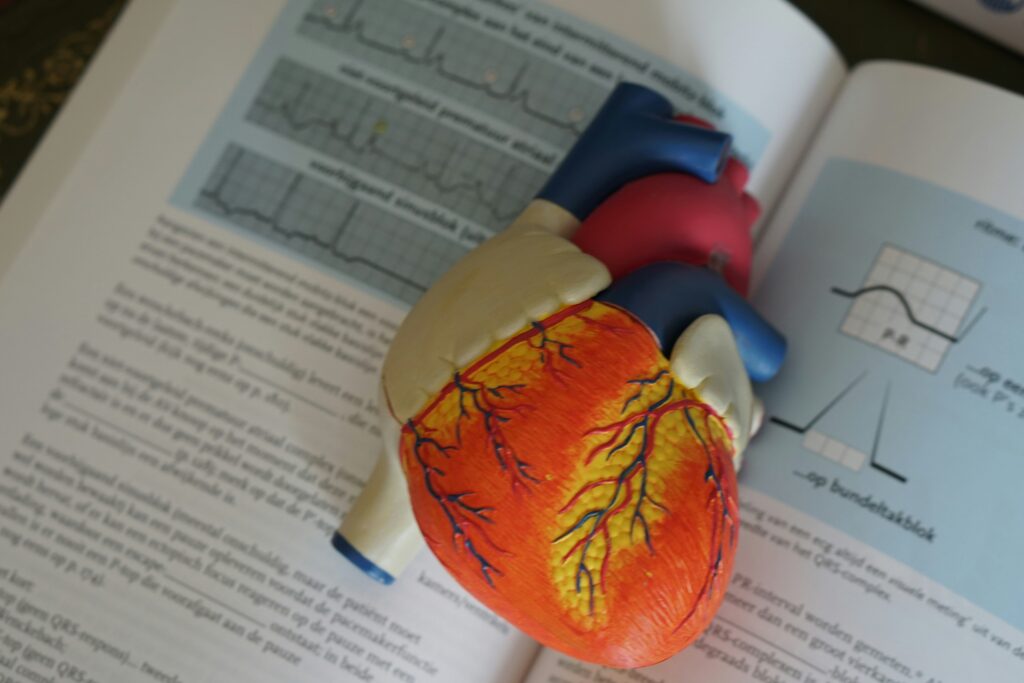
Coronary heart disease is one of the leading causes of death in Singapore. The coronary arteries provide blood and oxygen supply to the heart. Narrowing or blockage of the coronary arteries due to various causes can lead to ischemia (lack of blood flow) in the heart muscle, manifesting clinically as angina (chest pain).
Severe myocardial ischemia can cause a heart attack, affecting heart function and potentially leading to heart failure. Cultivating healthy lifestyle habits and correcting bad habits are important and our best shot at preventing heart diseases.
Here are the main symptoms of coronary heart disease.
1. Angina
It is characterized by chest pain, often pressing, tight, or burning, with the pain possibly extending to the neck and arms. Coronary heart disease can be difficult to detect, and even people who have annual check-ups may still develop it. “Some people take intermittent angina (also known as chest pain) lightly, but it is indeed a hidden danger of coronary heart disease.
2. Heart Attack
Also known as myocardial infarction or myocardial necrosis. The patient may experience severe chest pain accompanied by palpitations, nausea, vomiting, pallor, collapse, and fainting. If the condition reaches this point, it is already quite severe because once the myocardium dies, it cannot regenerate, and heart function will decline.
3. Silent Myocardial Ischemia
Many patients have extensive coronary artery blockages but almost never experience angina. Some even don’t feel angina during a myocardial infarction. In some cases, sudden cardiac death occurs, and routine medical checkups discover myocardial infarction only afterward.
4. Heart Failure and Arrhythmia
Some patients initially experience angina attacks, but due to widespread disease, myocardial fibrosis occurs, reducing or eliminating angina while heart failure manifests as symptoms such as shortness of breath, edema, and fatigue. Additionally, there are various arrhythmias, presenting as palpitations. Some patients never experience angina but present directly with heart failure and arrhythmia.
What are the risk factors for coronary heart disease?
1. Age: Men over 40 and women after menopause have an increased incidence of heart disease.
2. Smoking: Smoking is a significant risk factor for coronary heart disease and is also one of the easiest to avoid. Research has shown that in just 3 months of quitting smoking, the heart will show signs of recovery and in six months, your respiratory system will benefit from your smoke-free lifestyle.

3. Chronic diseases: Patients with hypertension, hyperlipidemia, and diabetes are in the high-risk group for coronary heart disease.
4. Obesity: Busy lifestyles have led to eating out more frequently and affluence has contributed to eating richer food – both factors leading to easier weight gain. Obesity is a risk factor for chronic diseases such as hypertension and hyperlipidemia.
Additionally, coronary heart disease is often associated with genetic predisposition, lack of exercise, heavy drinking, and high stress levels. Although not everyone with risk factors will develop coronary heart disease, people with these risk factors are 2-3 times more likely to get the disease than those without them.
What lifestyle changes can you make?
1. Make adjustments to your diet
The overall principle of diet is “four lows and two highs”: low salt, low sugar, low fat, and low calories; high vitamins and high fiber. Avoid overeating at each meal, pay attention to balanced nutrition, and control weight. Eat more whole grains and vegetables, fewer high-fat foods, and ensure adequate protein intake daily.
2. Control blood pressure
Epidemiological surveys show a direct relationship between hypertension and the incidence of stroke and coronary heart disease. In people aged 40-70, every increase of 20 mmHg in systolic blood pressure or 10 mmHg in diastolic blood pressure doubles their risk of cardiovascular events. Stable and effective blood pressure management can significantly reduce the risk of stroke and myocardial infarction. A target blood pressure of less than 130/90 mmHg is suitable. Common antihypertensive medications include diuretics, beta-blockers, calcium channel blockers, angiotensin-converting enzyme inhibitors, and angiotensin II receptor blockers.
3. Control blood sugar
Vascular damage is a chronic complication of diabetes, and high or unstable blood sugar can accelerate the development of atherosclerosis in the coronary arteries. Diabetic patients often have diffuse, multi-segment coronary artery disease, making medical, interventional, and bypass surgery less effective. Currently, commonly used antidiabetic medications include insulin and its analogs, sulfonylureas, metformin, alpha-glucosidase inhibitors, thiazolidinediones, meglitinides, GLP-1 receptor agonists, and DPP-4 inhibitors.
4. Control blood lipids
Blood lipids circulate in the blood in the form of lipoproteins, including chylomicrons, very low-density lipoproteins (VLDL), low-density lipoproteins (LDL), intermediate-density lipoproteins (IDL), and high-density lipoproteins (HDL). Among these lipoproteins, each has a different effect on atherosclerosis. Research shows that low-density lipoproteins lead to atherosclerosis, while high-density lipoproteins protect the heart. Therefore, when interpreting test reports, pay particular attention to LDL. Additionally, triglyceride-rich lipoproteins such as chylomicrons and VLDL themselves do not cause atherosclerosis, but their breakdown products may. Blood lipid control can be achieved through diet, medication, and exercise.

5. Quit smoking
Smoking poses severe risks to the cardiovascular system, with the harm correlated with the amount and duration of smoking. Compared to non-smokers, the time to the first heart attack is advanced by 10 years, and the risk of acute myocardial infarction increases sevenfold. For patients who have undergone stent implantation, smokers have a 1.55 times higher rate of re-narrowing, a 1.76 times higher relative risk of death, a 2.08 times higher risk of old myocardial infarction, and a more than threefold higher relative risk of sudden death.
6. Increase physical activity
Regular physical activity can reduce the risk of coronary heart disease. A retrospective study on the incidence of coronary heart disease in different occupations found that people with sedentary jobs had twice the rate of coronary heart disease compared to those with moderate physical activity. People who engage in moderate exercise have a 60% lower mortality rate from coronary heart disease.
7. Weight loss
Multiple studies show that the incidence of coronary heart disease is significantly higher in obese individuals than in those with normal body mass index, especially with an increase in abdominal fat.
The above factors are coronary heart disease risk factors that can be controlled through medication and lifestyle. By actively controlling them, the incidence of coronary heart disease can be managed. There are also factors that we cannot control, such as age (the older you are, the higher the incidence), gender (men have a significantly higher incidence than women), and genetics (coronary heart disease has a family genetic tendency).
Photo Credit:
Photo by DESIGNECOLOGIST on Unsplash
Photo by Robina Weermeijer on Unsplash
Photo by Reza Mehrad on Unsplash
Photo by Lucas van Oort on Unsplash
* Important: The information provided here is for general information purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a healthcare professional with any questions you may have regarding a medical condition.
